Authors: Whitaker, B. Brazos Valley Equine, Salado, Texas. Lowe, J. Innovative Medical Solutions Limited, Christchurch, New Zealand.
Contact author: Beau Whitaker – Beauwhitaker@gmail.com
CLINICAL RELEVANCE:
2.5% injectable Polyacrylamide Hydrogel (2.5% iPAAG) seems to have a tendency to integrate more readily with damaged or inflamed synovial tissue compared to healthy tissue.
This could explain its excellent safety profile and provide a rationale for targeted therapy in patients with osteoarthritis, as well as its use in treating DFTS injuries in horses.
INTRODUCTION:
2.5% iPAAG has emerged as a significant innovation in equine sports medicine worldwide for managing osteoarthritis (OA)1. The 2.5% iPAAG, commercially known as Arthramid® (Contura, Denmark), has distinct physical and biological properties that make it effective in tissue applications, particularly in synovial joints1.
This study evaluates the histopathologic effects of 2.5% injectable polyacrylamide hydrogel (2.5% iPAAG) within the digital flexor tendon sheath (DFTS) of a 17-year-old paint gelding. The DFTS is a synovial structure that encases the deep digital flexor tendon (DDFT) and is critical for the smooth gliding of tendons during limb movement2.
It consists of the synovial membrane, the manica flexoria, and the tendon itself, which are essential for maintaining tendon health and function.
Despite the documented clinical benefits in treating OA, the exact nature of the interaction between 2.5% iPAAG and the synovium and non-synovial soft tissues within the DFTS have not been thoroughly investigated. This study aims to fill this gap by assessing how 2.5% iPAAG interacts with damaged and fibrillated tendon tissues exposed to the synovium in the DFTS, which has significant implications for healing and treatment timing.
MATERIALS AND METHODS:
A terminal case study was conducted on a systemically healthy horse with no pre-surgical soft tissue pathology in the DFTS. Under general anesthesia, a beaver blade was used to create a lateral incision into the deep digital flexor tendon (DDFT) and the lateral aspect of the manica flexoria on both forelimbs, followed by debridement with a synovial resector. Two weeks post-surgery, 2ml (50mg) of 2.5% iPAAG was injected into the left forelimb’s DFTS, the right limb acting as control.
Clinical lameness examinations and ultrasound evaluations were performed weekly and bi-weekly, respectively until 60 days post-surgery when the horse was humanely euthanised and tissue samples collected and fixed for histopathologic evaluation of the DFTS synovium, manica flexoria, and DDFT of both forelimbs.
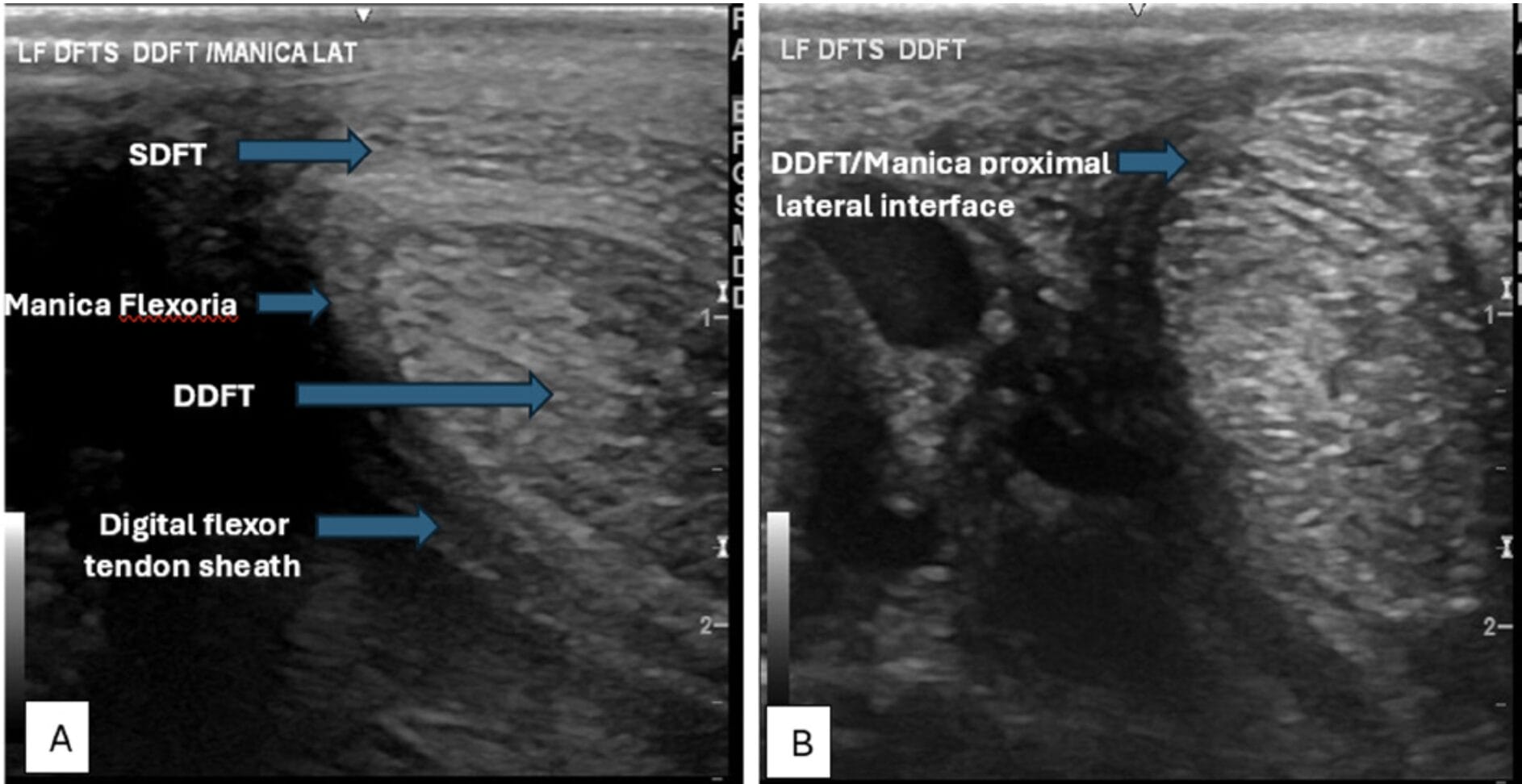
Figure 1A: Ultrasound image showing the anatomy of the structures of the left front lateral digital flexor tendon sheath pre surgery. 1B: 30 days post-surgery at the level created lesion showing damage within the lateral surface of the DDFT and the manica flexoria.
RESULTS:
At 60 days post-surgery (45 days post treatment), no 2.5% iPAAG was detected in the damaged DDFT or manica flexoria of the treated left limb. Instead, the gel had integrated into the inflamed synovial surface and extracellularly in the synovial space at the DDFT/manica interface where the surgical lesions were created. The gel’s presence was notably absent in non-inflamed synovium. There was no difference in histopathologic appearance of the DDFT or manica between the left and right forelimbs.
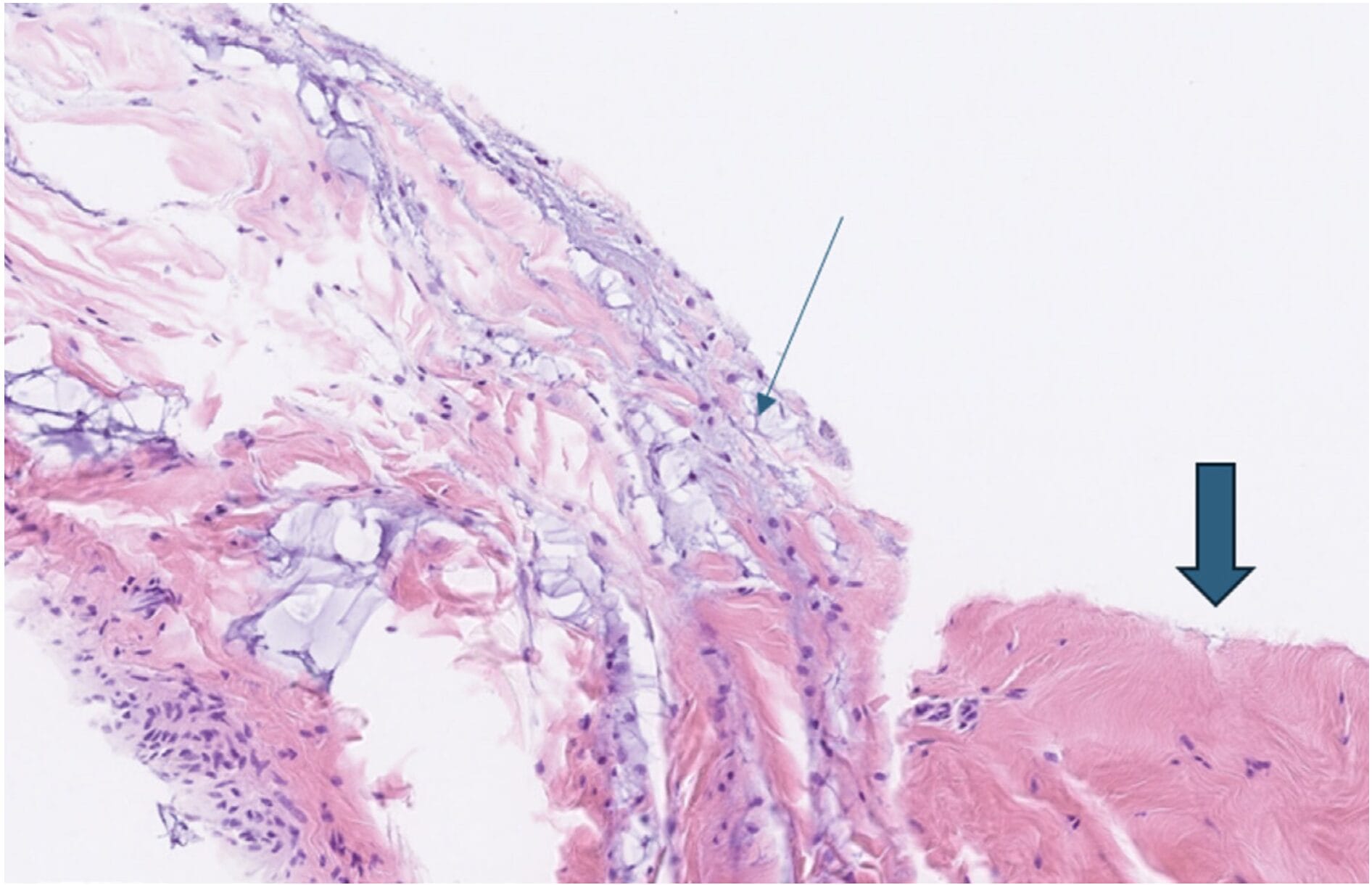
Figure 2: Left lateral DDFT inflamed synovial surface with small amounts of light blue gel (small arrow) 45 post intra synovial injection of 2.5% iPAAG. Note the lack of blue gel present in the non-inflamed synovium (large arrow).
DISCUSSION:
The findings imply that while 2.5% iPAAG does not incorporate with damaged tendon fibres, it preferentially associates with inflamed synovium, potentially serving as a protective barrier and aiding in the management of inflammation, which is known to delay the healing of DFTS injuries and contribute to the ongoing clinical signs of lameness2.
This interaction is likely a response to increased cellular activity in the damaged area, facilitated by the gel’s ability to exchange water molecules with host tissue3,4 rather than being primarily influenced by random factors such as gravity, biomechanics, or fluid dynamics. This targeted interaction may also help prevent adhesion formation and reduce inflammation in both the synovium and synovial fluid, consistent with anecdotal reports of success in treating synovitis and chronic soft tissue injuries within the DFTS.
CONCLUSION:
This study provides valuable insights into the interactions of 2.5% iPAAG within the equine DFTS, highlighting its potential role in enhancing tendon sheath healing and function. It also paves the way for further research into its application in the treatment of osteoarthritis from its targeted therapeutic effect on damaged synovium.
References
1. Tnibar A. (2022) Intra-articular 2.5% polyacrylamide hydrogel, a new concept in the medication of equine osteoarthritis: a Review. J Equine Vet Sci. 119:104143. doi:10.1016/jevs.2022.104143
2. Smith R. (2024) Treatment of tendinopathies. Equine Vet Edu. 36 (12):659-72. Published 2024 June 06. doi.org/10.1111/eve.13987
3.Christensen L, Camitz L, Illigen K.E, Hansen M, Sarvaa R and Conaghan P,G. (2016) Synovial incorporation of polyacrylamide hydrogel after injection into normal and osteoarthritic animal joints. Osteoarthr. Cartil. 24, 1999–2002. http:// dx.doi.org/10.1016/j.joca.2016.07.007. Accessed August 13, 2020
4. Lowe J, Clifford L, Julian A, Koene M. (2024) Histologic and cytologic changes in normal equine joints after injection with 2.5% injectable polyacrylamide hydrogel reveal low-level macrophage-driven foreign body response. J Am Vet Med Assoc. 262 (5):649-647. Published 2024 Feb 21. doi:10.2460/javma.23.10.0553


